China3D printingNet August 28, researchers from Lawrence Livermore National Laboratory (LLNL) will3D bioprintingCombined with computational process simulation to better understand the spread of cancer during metastasis.
Together with scientists from Duke University, the team injected tumor cells into3D printingStructure of brain cells. By performing hydrodynamic analysis of the process, the team was able to determine where the tumor is attached, paving the way for potential predictive models. Using researchers’ novel computer-based modeling methods, future clinicians can predict the spread of cancer cells in individual patients.
Monica Moya, the lead researcher of LLNL research, said: “Computational modeling is definitely a useful tool, but you still need to benchmark it with real things. With this method, we can verify The need for models makes biology simple and clean, and can increase the complexity of biological and computational models.
For physical issues in biology, this paper does provide a framework, because how you can use these models in in vitro models and perform simulations to truly enhance the strength of the field. “
3D printing
Patterns in the structure of blood vessels” alt=”Computer analysis performed at LLNL revealed that cancer cells are clustered in
3D printing
The pattern in the structure of blood vessels” width=”620″ height=”354″ />
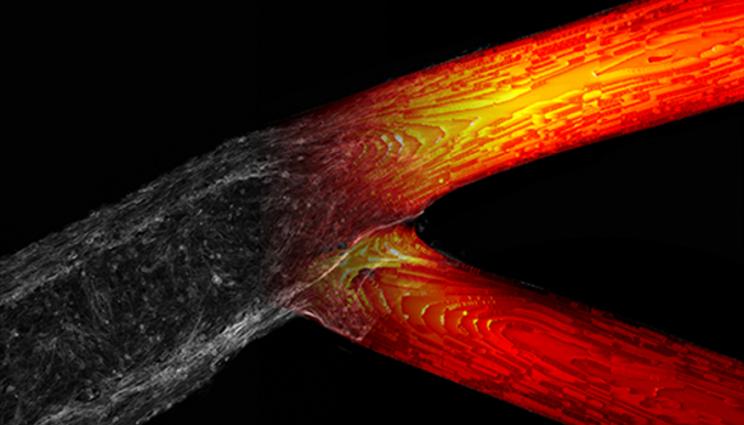
Computer analysis performed at LLNL revealed that cancer cells are clustered in3D printingPattern in the structure of blood vessels. Picture from LLNL.
urgent need3D printingCancer solutions
For more than 150 years, people have known that cancer cells can invade secondary sites and cause tumors, but it is still impossible to predict the exact trajectory of these growths. Doctors currently cannot locate and treat cancers early, which makes them difficult to treat, and when growths occur in the brain, they are almost always fatal.
Moya described the process of cancer cells spreading, attaching and growing on the walls of blood vessels, just like planting seeds in soil. MoyaExplains: “Tumor cells tend to escape from the primary tumor and spread through the vasculature. They eventually attach to the walls of blood vessels, penetrate the endothelium into tissues, and grow like seeds in the soil.”
Due to the large number of differentiation factors between each vascular system in the study, it is almost impossible to further understand where the cells landed through research. Measuring mechanical forces (for example, dynamic fluid flow in the body) also requires greatly simplifying existing test models, which limits their usefulness in drawing conclusions.
Although a large number of previous studies on cancer growth have involved computer modeling, it is important to verify these hypotheses through in-situ testing. If proven correct, these theories will be the key to understanding the role of flow patterns, vessel geometry, and tissue compliance in intravascular seeding. Therefore, having highly detailed models is essential to take full advantage of the insights of cancer research.
Despite the importance of verification, methods are usually limited to the use of microfluidic devices, which do not have tubular channels or vascular compliance, which are two important features of in vivo models. Microfluidic devices also lack all the attachment sites available for circulating tumor cells (CTC), and their geometry cannot be accurately replicated between models.
The vascular structure of the LLNL team showed the same storage modulus as real human brain tissue. Picture from LLNL.
LLNL team hydrogel-based equipment
In order to overcome the limitations of existing microfluidic devices, the LLNL team developed a hydrogel-based vascular flow device.Utilize customized extrusion-based3D printingMachine, the sacrificial bio-ink can be patterned and then embedded in the gelatin fibrin hydrogel. Then empty the light channel and inject immortalized human brain endothelial cells to form blood vessel-like tissue.
Although a variety of vascular geometries can be achieved using hydrogels, the researchers initially chose to create simplified straight and branched geometries. By starting with the basic structure, the team aims to draw broader conclusions based on the many continuous small changes in the testing process. The blood vessels are generally the size of small arteries, with two 45° stratified branch points, and the diameter of the sub-vessels is getting smaller and smaller.
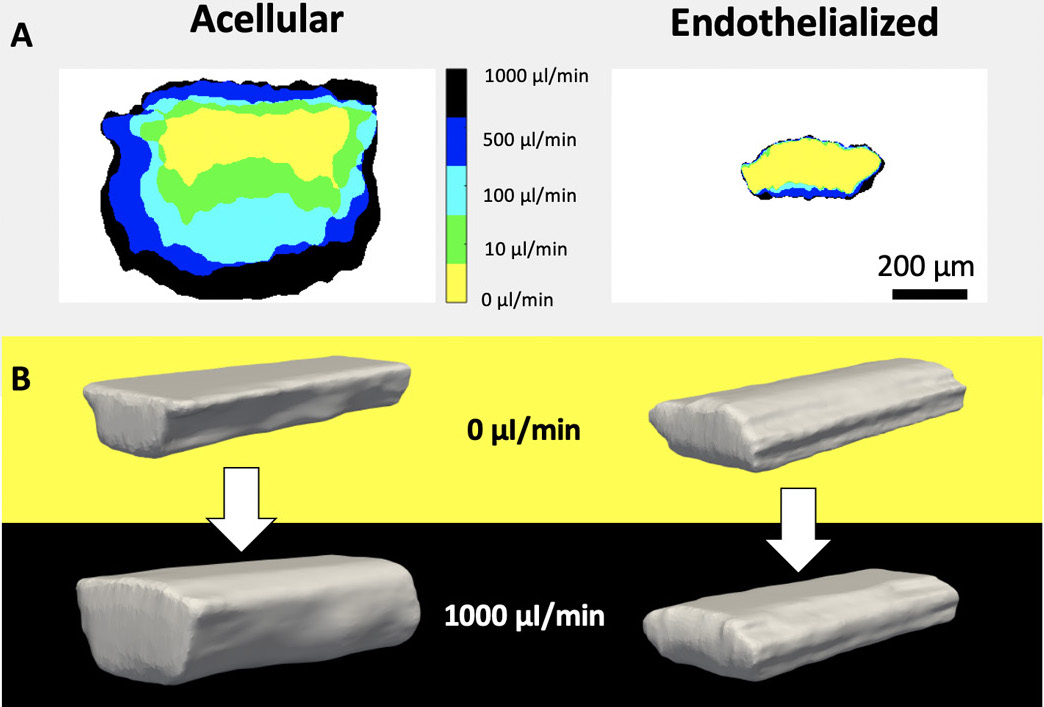
To test its additional vascular system, the LLNL team connected it to a pneumatic fluid supply system. After 7 days, endothelial cells completely covered all exposed channel surfaces, forming a confluent layer of the endothelial lining. Subsequently, a series of flow rate tests were performed on the vessel and imaged with a confocal microscope to evaluate its response to changing flow rates.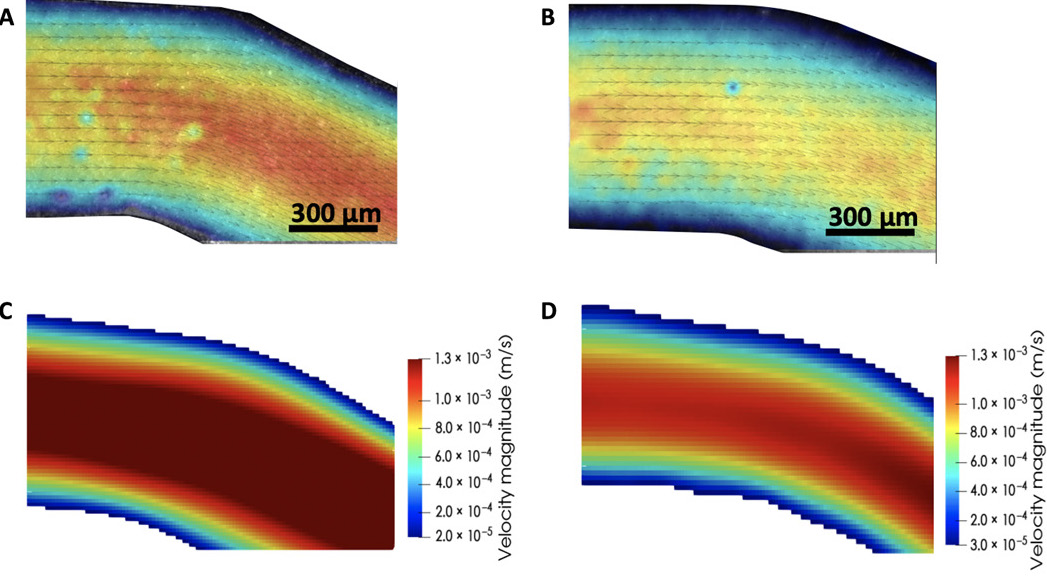
The researchers concluded that their combined verification method has successfully found a pattern of cancer cell behavior. Picture from LLNL.
It is found that the final storage modulus of the gel is similar to the storage modulus reported in human brain tissue, so it is very suitable for testing the possibility of CTC attachment. The metastatic breast cancer cells were filtered and circulated through the bioprinting device at an average flow rate of 1690 μl/min for 1 hour. Then fix the device, dye and image to determine the connection position of the CTC.Tests have shown that CTC tends to attach it to the branch point of the vessel rather than its straight part.Continuous analog display3D printingThe arterial wall shear stress (WSS) level is also an important factor in the adhesion rate. Although greater shear stress was applied to cancer cells in a straight channel, it was found that the higher WSS observed in a smaller area can enhance its anchoring effect.Based on their findings, the LLNL team concluded that their strategy of performing increasingly complex computational fluid dynamics simulations has been successful. Researchers believe their method is the first step in using computational models to determine how cancer cells spread to distant organs.
China3D printingInternet Comment: Using this method, we can test, observe and measure biological phenomena that were impossible before. By pairing our engineering platform with a computational model, we can directly inquire about the behavior of metastatic cells and the rules for controlling metastatic cells, which is much faster than conducting experiments alone. “
use3D printingFight cancer
Researchers often use additive manufacturing as a way to discover more cancer cells, with the ultimate goal of finding a way to fight deadly diseases.Scientists from Nagoya City University in Japan have developed a new type of3D printingCancer drug delivery system. The team used polymer hydrogels to create implantable patches that were proven to carry liposomal doxorubicin drugs.
An assistant professor at Virginia Commonwealth University has used3D printingCreated a real-time model of tumor cells. This breakthrough could allow cancer researchers to better understand the progression of the disease.
Researchers from the United States and Germany have produced glioblastoma (GBM) (a type of aggressive brain cancer)3D bioprintingModel. Biologically manufactured cell structures may help clinicians better understand this disease and accelerate the discovery of new drugs to combat this disease.
China3D printingNet compile article!
(Editor in charge: admin)

0 Comments for “LLNL scientists use biological 3D printing technology to understand the spread of cancer”