Rice University
biology
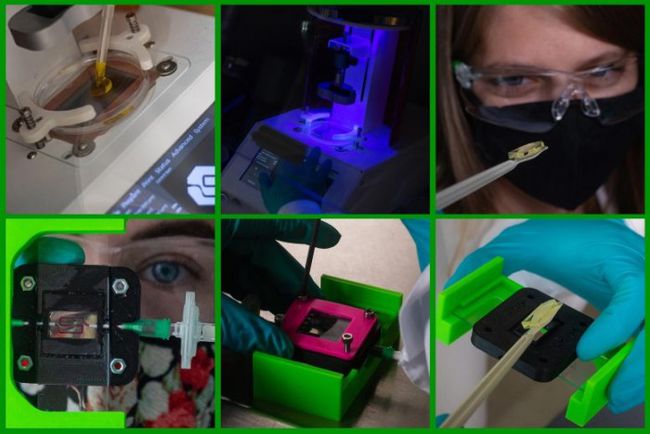
Engineers are using3D printingAnd smart biomaterials to create an insulin-producing type for patients with type 1 diabetes
Implants
.This three-year project is a collaborative project between Omid Veiseh and Jordan Miller’s laboratories.
Funding
Supported by JDRF. Veiseh and Miller will use insulin-secreting beta cells made from human stem cells to create an implant that senses and regulates blood sugar levels by responding to the correct amount of insulin at a specific time.
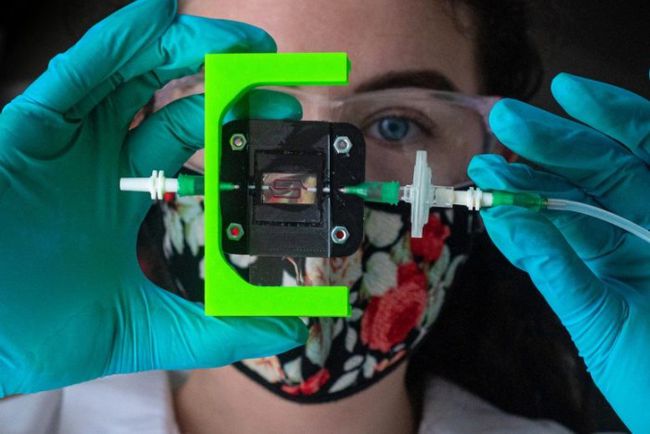
Veiseh, an assistant professor of bioengineering, has spent more than ten years developing biomaterials to protect implanted cell therapy from the immune system.Miller, an associate professor in the Department of Bioengineering, has spent more than 15 years researching3D printingWith
Blood vessel
(Or vascular network) organization technology.
Veiseh said: “If we really want to reproduce the normal function of the pancreas, we need the vascular system. This is the purpose of this grant in cooperation with JDRF. The pancreas naturally has all these blood vessels, and the cells are organized in a special way in the pancreas. . Jordan and I want to print in the same direction that exists in nature.”
Type 1 diabetes is an autoimmune disease that causes the pancreas to stop producing insulin, the hormone that controls blood sugar levels. Approximately 1.6 million Americans have type 1 diabetes, and more than 100 cases are diagnosed every day. Type 1 diabetes can be controlled by injecting insulin. However, it is difficult to balance insulin intake with diet, exercise, and other activities. Research estimates that in the United States, less than one-third of type 1 diabetes patients can consistently reach their target blood sugar levels.
The goal of Veiseh and Miller is to demonstrate that their implants can properly regulate blood sugar levels in diabetic mice for at least 6 months. To do this, they need to give their engineered beta cells the ability to respond to rapid changes in blood sugar levels.
Miller said: “We must keep the implanted cells close to the blood so that the beta cells can sense and quickly respond to changes in blood sugar.” He said that ideally, insulin-producing cells are no more than 100 microns away from blood vessels. Miller said: “We use advanced3D bioprintingThe combination of technology and host-mediated vascular remodeling gives each implant a chance to bind to the host.
Insulin-producing cells will be protected by a hydrogel formulation developed by Veiseh, who is also a scholar at the Texas Cancer Prevention and Research Institute. This hydrogel material has been proven to effectively encapsulate the cell therapy method in a bead-sized sphere, with pores small enough to prevent the cells from being attacked by the immune system, but large enough to provide nutrients and sustain life. Insulin passes.
“The blood vessels can enter it,” Veiseh said. “At the same time, we have our coating, our small molecules, which prevent the body from rejecting the gel. Therefore, it should be very coordinated with the body. “
If the implant responds too slowly to high or low blood sugar levels, this delay can have a roller coaster-like effect, that is, insulin levels repeatedly rise and fall to dangerous levels.
“Solving this delay is a huge problem in this area,” Veiseh said. “When you challenge mice-and ultimately humans-a glucose that mimics eating, how long does it take for this information to reach our cells, and how does insulin come out quickly?” With the addition of blood vessels, he and Miller hope to make their β-cell tissue behave more closely to mimic the natural behavior of the pancreas.
(Editor in charge: admin)

0 Comments for “Scientists use 3D printing and smart biomaterials to make insulin-producing implants for patients with type 1 diabetes”